Uterine fibroids, also known as leiomyomas or myomas, are benign tumors that develop in the muscular layer of the uterus (myometrium). These tumors are quite common, with studies indicating that up to 70-80% of women may develop fibroids by the age of 50. While they are typically non-cancerous, they can lead to various symptoms and complications that require medical attention.
Formation of Uterine Fibroids
Pathophysiology:
The exact cause of uterine fibroids remains unclear, but several factors are believed to contribute to their formation. Hormonal influences, particularly estrogen and progesterone, play a significant role in their growth. These hormones stimulate the proliferation of smooth muscle cells in the uterus, leading to the development of fibroids.
1. Genetic Factors: Research suggests that genetics may predispose certain individuals to develop fibroids. Specific gene mutations have been identified in fibroid tissues, indicating a hereditary component. Women with a family history of fibroids are more likely to experience them.
2. Hormonal Influence: Fibroids often enlarge during periods of high estrogen levels, such as pregnancy, and may shrink after menopause when hormone levels decrease. This suggests that fibroids are sensitive to hormonal changes.
3. Growth Factors: Several growth factors, such as insulin-like growth factor (IGF), may also play a role in fibroid development. These factors can stimulate cell growth and proliferation, contributing to the increase in fibroid size.
4. Other Factors: Lifestyle factors such as obesity, diet, and stress may indirectly influence the development of fibroids. Obesity, for instance, is associated with increased estrogen production, which may promote fibroid growth.
Types of Uterine Fibroids
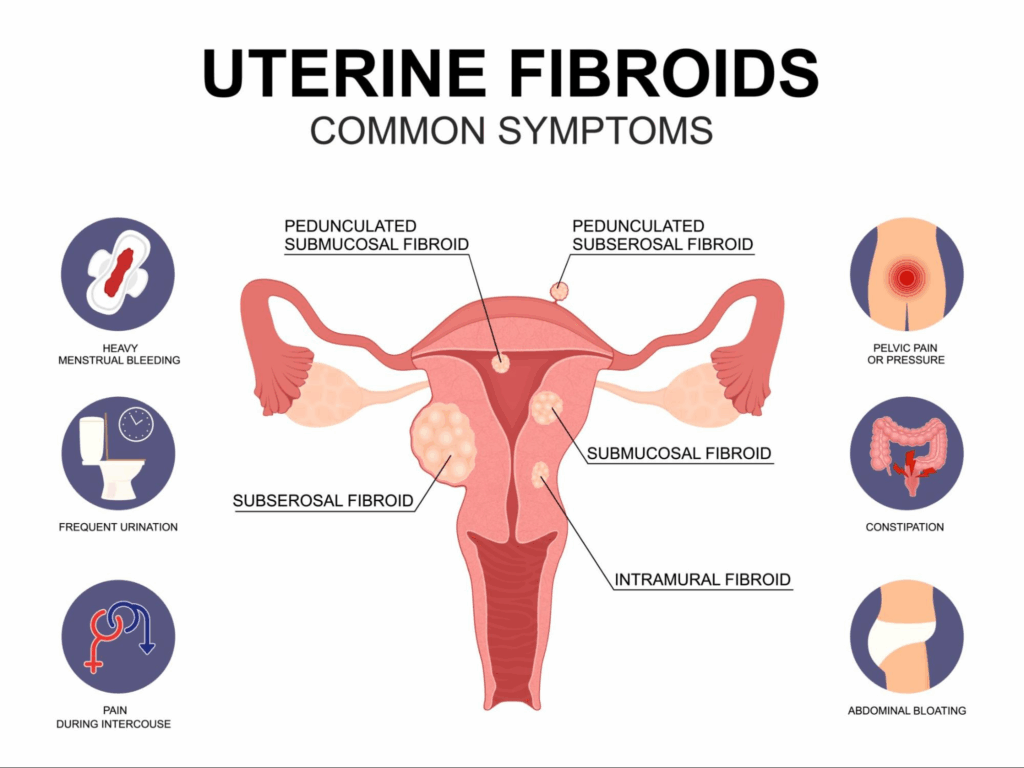
Uterine fibroids can vary in size, number, and location. The main types include:
– Intramural Fibroids: These are the most common type, located within the uterine wall.
– Subserosal Fibroids: These protrude from the outer surface of the uterus and can be large.
– Submucosal Fibroids: These grow just beneath the lining of the uterus and can protrude into the uterine cavity.
– Pedunculated Fibroids: These are attached to the uterus by a stalk and can be either subserosal or submucosal.
Symptoms of Uterine Fibroids
While many women with uterine fibroids experience no symptoms, those who do may present with a variety of issues. The severity of symptoms often correlates with the size, number, and location of the fibroids.
Common Symptoms
1. Menorrhagia: One of the most common symptoms is heavy menstrual bleeding. Women may experience prolonged periods with excessive bleeding, leading to anemia and fatigue.
2. Pelvic Pain: Fibroids can cause significant pelvic discomfort or pain. This pain may be chronic or acute, depending on the fibroid’s size and location.
3. Pressure Symptoms: Large fibroids can exert pressure on surrounding organs, leading to symptoms such as frequent urination, difficulty emptying the bladder, or constipation.
4. Reproductive Issues: Fibroids can impact fertility and pregnancy. They may interfere with implantation or cause complications such as miscarriage or preterm labor.
5. Abdominal Distension: Women may notice an increase in abdominal girth or a feeling of fullness, similar to having a growing abdominal mass.
Additional Symptoms
– Back Pain: Some women report lower back pain, which may be attributed to the pressure exerted by fibroids.
– Pain During Intercourse: Fibroids located near the cervix or vaginal wall may cause pain during sexual activity.
– Bloating: Many women experience bloating or a feeling of fullness in the abdomen.
– Mood Changes: Chronic pain and heavy bleeding can contribute to anxiety and depression in some women.
Diagnosis
Diagnosis of uterine fibroids typically involves a combination of medical history, physical examination, and imaging studies. Healthcare providers may perform:
1. Pelvic Exam: During a routine pelvic examination, the doctor may feel for abnormalities in the uterus.
2. Ultrasound: A transvaginal or abdominal ultrasound can help visualize fibroids and assess their size and location.
3. MRI: In some cases, magnetic resonance imaging (MRI) may be used for a more detailed view of the fibroids.
4. Hysteroscopy: This procedure involves inserting a thin, lighted tube through the vagina and cervix into the uterus, allowing direct visualization of fibroids.
Treatment Options
Treatment for uterine fibroids depends on the severity of symptoms, the size and location of the fibroids, and the woman’s reproductive plans. Options include:
1. Watchful Waiting: If fibroids are small and asymptomatic, a “watch and wait” approach may be adopted.
2. Medications: Hormonal therapies can help manage symptoms. For instance, hormonal contraceptives may regulate menstrual cycles, while gonadotropin-releasing hormone (GnRH) agonists can shrink fibroids temporarily.
3. Surgical Options:
Myomectomy: This surgical procedure involves the removal of fibroids while preserving the uterus, suitable for women who wish to maintain fertility.
Hysterectomy: For severe cases, particularly in women who have completed their family, a hysterectomy may be recommended to remove the uterus entirely.
4. Minimally Invasive Procedures: Techniques such as uterine artery embolization (UAE) can reduce blood flow to fibroids, causing them to shrink.
Uterine fibroids are prevalent among women and can significantly impact quality of life. Understanding their formation and symptoms is crucial for early diagnosis and appropriate management. Women experiencing symptoms should consult healthcare providers to discuss potential treatment options and maintain reproductive health. As research into fibroids continues, advancements in treatment and understanding of their etiology will likely improve outcomes for those affected.
For women dealing with uterine fibroids, it’s essential to approach the decision regarding surgery thoughtfully. While surgical options such as myomectomy and hysterectomy can effectively alleviate symptoms, they should not be the first line of treatment. Non-invasive methods and medication often provide satisfactory symptom relief without the risks associated with surgery. However, if symptoms are severe or persistent, surgical intervention may become necessary. In Hong Kong, the costs for surgeries can vary significantly: myomectomy typically ranges from HKD 50,000 to HKD 100,000, while hysterectomy can cost between HKD 80,000 and HKD 150,000. It’s crucial to consult with a healthcare provider to explore all options, understand the financial implications, and ensure that surgery is the most appropriate choice based on individual circumstances. Taking the time to weigh these factors can lead to more informed and beneficial health decisions.