A new study published in the journal Current Directions in Psychological Science has revealed that mitochondria, the tiny energy factories inside brain cells, may be the missing link between stress, trauma, and mental health. These microscopic powerhouses not only generate energy but also seem to translate emotional experiences into biological changes that shape how we feel and think.
Mitochondria: The Hidden Translators Of Stress
For decades, researchers have understood that experiences such as chronic stress, loneliness, and trauma can alter brain function. What remained unclear was how these external pressures become internal biological reactions. According to Christopher Fagundes, professor of psychological sciences at Rice University,
“We actually have biomarkers that really are showing links between psychological processes and people’s physiology.”
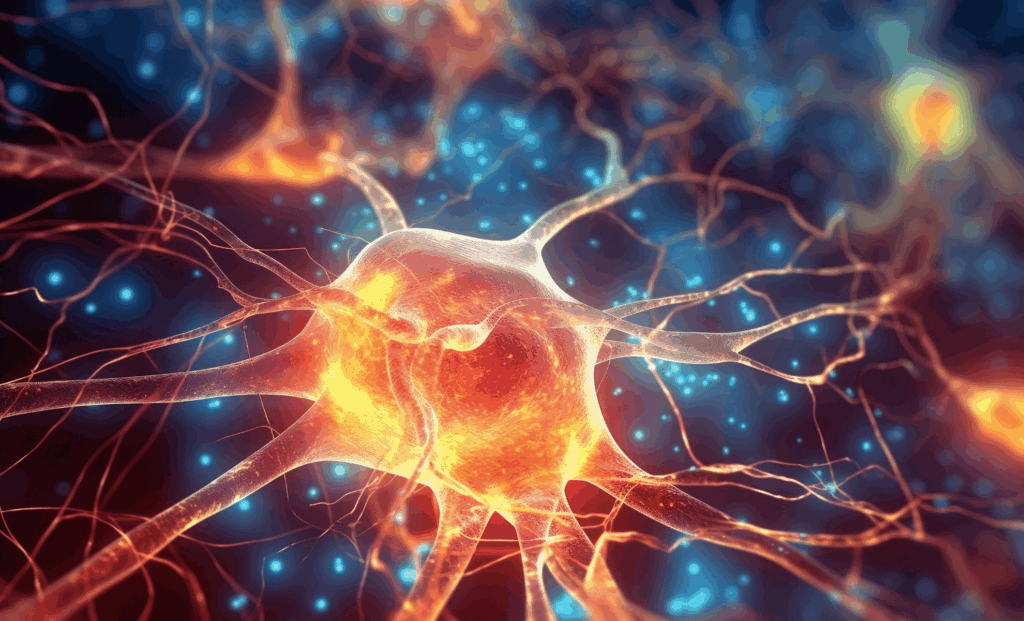
At the center of this biological bridge are mitochondria, often called the “engines” of our cells. They not only produce ATP—the body’s primary energy currency—but also help regulate immune responses, inflammation, and neural signaling. When exposed to prolonged stress, mitochondria lose efficiency, impairing energy flow throughout the brain and body.
“The actual cellular machinery that links these experiences to disease really starts at the level of the mitochondria,” said Fagundes.
This means the same organelles that fuel thought and emotion may also determine how psychological wounds manifest as physical illness.

Credit: Current Directions in Psychological Science
Why Mental Health Depends On Cellular Energy
The human brain consumes an extraordinary share of the body’s energy. Every thought, memory, or emotional reaction depends on seamless mitochondrial performance. When these organelles falter, neural transmission slows, synaptic flexibility declines, and mood regulation suffers. Variations in mitochondrial DNA have been tied to heightened risks for anxiety, depression, and cognitive impairment.
Researchers are now recognizing that even subtle mitochondrial changes can set off cascades of dysfunction.
“A lot of the relationships that we’ve been thinking of – [between] inflammatory processes and these kinds of mental health outcomes – we should look toward alterations in mitochondria being a real mediator or [underlying] mechanism,” Fagundes explained.
How Stress And Isolation Rewrite The Body’s Energy Code
Chronic stress doesn’t merely affect mood—it reshapes metabolism. Over time, stress pushes mitochondria into an inefficient state, producing fewer energy molecules and more inflammatory signals. This biological imbalance can feel like fatigue, brain fog, or emotional instability. The study, published in Current Directions in Psychological Science, emphasizes that mitochondria sit at the center of these pathways, bridging mental distress and physical health outcomes.
Fagundes also highlighted the toll of social isolation on mitochondrial vitality.
“When people are lonely and socially isolated, a lot of times there seems to be this loop where they have more anxiety to go out of the house,” he noted.
“That is a recipe for negative alterations in the mitochondria, less energy, less resources to expend. So, when one does try to break that cycle, it’s much more difficult.”
This vicious feedback loop between energy depletion and emotional withdrawal underscores how biology and behavior intertwine in mental health struggles.
Restoring The Brain’s Cellular Resilience
Fortunately, mitochondria are remarkably adaptable. Lifestyle changes and therapeutic interventions can restore their efficiency and even increase their number. Aerobic exercise, for instance, boosts mitochondrial enzyme activity and promotes biogenesis, the creation of new mitochondria. These changes enhance neural communication and mood stability, providing a biological explanation for why regular movement improves mental health.
Early findings suggest that mindfulness practices and psychotherapy may also strengthen mitochondrial performance. Studies show that trauma-focused therapy for PTSD can increase mitochondrial density, even if symptom relief takes time to follow.
“We’ve been talking a lot about things like inflammation. It tells us something is happening, but mitochondria help us explain why it’s happening at the cellular level,” Fagundes said. “If we focus more at the cellular level, we’ll have a much deeper understanding of underlying processes.”