The persistent hum, hiss, or ring of tinnitus—often described as a phantom sound—is not just a sensory glitch. For more than 250 million people globally, it’s an unrelenting companion that reshapes daily life. From mild irritation to full-blown sleep disruption and anxiety, the condition is often treated as untouchable: poorly understood, difficult to diagnose, and impossible to cure.
But that assumption is beginning to shift. New research from the University of Oxford has unearthed a surprising connection between tinnitus and one of the body’s most fundamental systems: sleep. Specifically, the patterns of neural activity that drive deep sleep may also act as a natural suppressor of tinnitus-related brain signals.
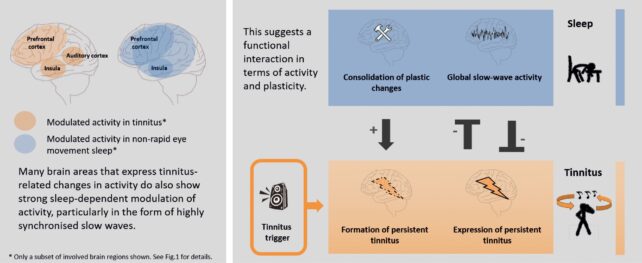
At the center of this research is a radical reframe of tinnitus—not as a static condition of the ear, but as a dynamic brain state that shifts depending on the body’s internal rhythms. That premise could open the door to a new class of therapies rooted not in external interventions, but in the body’s own architecture.
Sleep, the Brain’s Quiet Regulator
The latest findings, published in Brain Communications, focus on non-REM (NREM) sleep, the phase characterized by slow-wave brain activity critical for cognitive recovery. These deep-sleep rhythms appear to directly counteract the hyperactive neuronal firing linked to tinnitus.
In a 2022 review and a follow-up animal study led by Linus Milinski of Oxford’s Sleep and Circadian Neuroscience Institute, researchers observed ferrets after exposure to loud noise. Those that developed tinnitus also showed disrupted sleep patterns and signs of overactive brain responses to sound stimuli.
“We could actually see these sleep problems appear at the same time as tinnitus after noise exposure,” Milinski said. “This suggested, for the first time, a clear link between developing tinnitus and disrupted sleep.”
During episodes of deep NREM sleep, the abnormal hyperactivity in the auditory cortex was significantly dampened. When the animals remained awake or slept lightly, the tinnitus-related signals persisted—indicating that sleep may suppress or modulate tinnitus activity in the brain.
Another study from South China University of Technology, cited by Milinski in ScienceAlert, found similar patterns in human participants. Researchers noted that individuals with tinnitus were less able to suppress brain hyperactivity as they transitioned into sleep. During deep sleep, however, the abnormal activity was markedly reduced.
A Neurological Loop With No off Switch
The implications of these findings go far beyond the lab. Clinical evidence supports a pattern that tinnitus and sleep disorders frequently co-occur—and may reinforce each other.
A 2023 study published in the International Archives of Otorhinolaryngology examined patients with chronic tinnitus and found that over 72% rated their sleep quality as poor. More than a quarter experienced moderate insomnia, and a significant correlation was found between tinnitus severity and sleep disruption.
Another independent study in Medicine (Baltimore) reported similar findings: patients with more severe tinnitus experienced greater insomnia symptoms, although no strong link was found to daytime sleepiness or risk of sleep apnea.


According to Milinski, “Tinnitus can make sleep worse, and poor sleep may, in turn, make tinnitus worse. It may be a kind of vicious circle, although I do not believe it is unbreakable.” This quote is taken directly from RNID’s research page, where Milinski outlines the research goals and early findings.
The idea that tinnitus may represent “local wakefulness” during sleep—a state where certain brain regions remain active while others are shut down—has also been proposed in a report from Oxford’s Department of Physiology, Anatomy and Genetics. This mismatched brain state may prevent restorative deep sleep and allow tinnitus-related activity to persist, even as most of the brain rests.
Reframing Tinnitus as a Brain Rhythm Disorder
For decades, tinnitus has been viewed through a peripheral lens—as a consequence of ear damage or age-related hearing loss. But the research now points to a more central problem: cortical hyperactivity, particularly in the auditory cortex, driven by abnormal neural feedback loops.
This aligns with a broader theory in neuroscience that phantom percepts like tinnitus stem from dysregulated spontaneous activity in the brain. In this framework, tinnitus is not just a reaction to silence but a maladaptive brain prediction, continually generating sound in the absence of real stimuli.
The Oxford-led review in Brain Communications introduces a new model: by amplifying or supporting deep sleep, it may be possible to interrupt this pathological loop and rebalance the brain’s auditory pathways. The researchers propose that enhancing slow-wave activity, either naturally or through non-invasive neurostimulation, could become a therapeutic pathway for future treatment.
Timing and Intervention
If confirmed through large-scale studies, these insights could change how tinnitus is treated—and when. Milinski and his team believe that early intervention—in the hours or days after tinnitus onset—could prevent it from becoming chronic, particularly if sleep is supported during this period.
“Widening the scope in tinnitus research towards the brain’s natural dynamics will provide fruitful ground for understanding those of pathological nature,” Milinski said in Oxford’s official research statement.
Future research will aim to identify neurophysiological markers of tinnitus during sleep and test methods to reinforce deep-sleep brain activity. The goal is not just to mask tinnitus, but to interrupt the brain’s faulty feedback loop at its source.

