The experimental technology, developed by Science Corporation, combines a chip thinner than a human hair with augmented reality glasses—and it’s already changed lives across Europe.
At the heart of this medical breakthrough is the PRIMA system, a photovoltaic retinal implant paired with AR glasses. In a recent clinical trial involving 38 patients, 80% recovered enough central vision to identify letters and words—a first for those suffering from geographic atrophy, the most advanced stage of dry AMD, according to the trial published in The New England Journal of Medicine.
This condition affects around five million people globally, often robbing them of the ability to perform basic visual tasks. The currently approved treatments, pegcetacoplan and avacincaptad, can only slow the disease. This new approach represents a different kind of progress: not preservation, but restoration. For patients like Sheila Irvine, who once thought she’d never read another book, the difference is transformative. “It was dead exciting when I began seeing a letter,” she shared in a statement from Moorfields Eye Hospital.
How the Implant Rewires the Eye to See
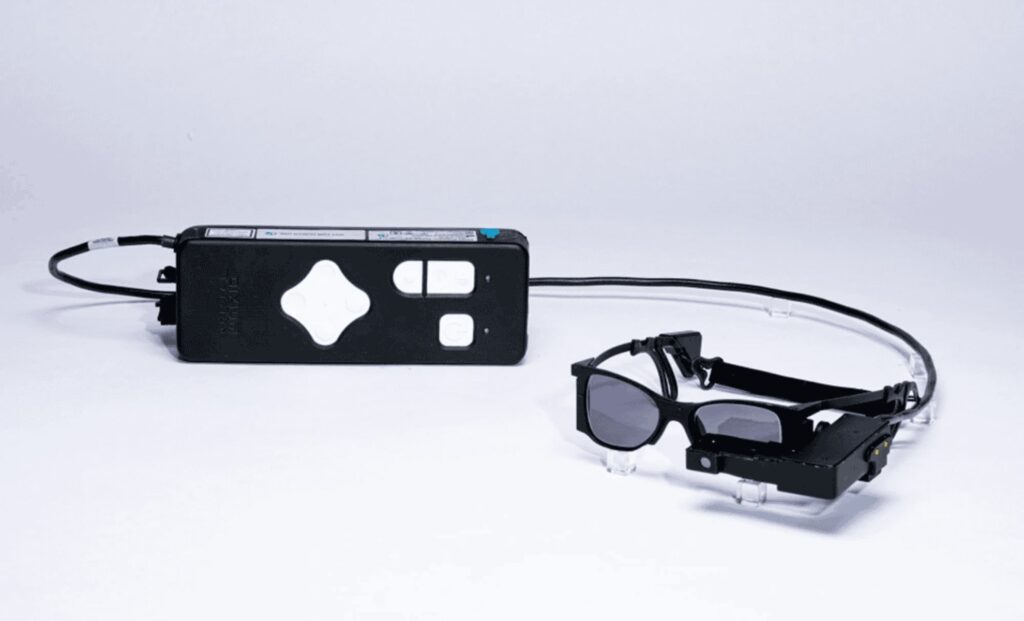
The PRIMA implant, developed in Paris by Pixium Vision and now backed by Science Corporation, is a two-millimeter-wide chip that works like a solar panel under the retina. It doesn’t require a battery or wires, instead running entirely on near-infrared light beamed in from the custom AR glasses worn by patients.
These glasses are connected to a waist-worn pocket computer that captures real-world images through a front-facing camera. According to Nature, the images are then converted into light pulses that stimulate remaining retinal neurons, allowing the brain to receive signals once again from the previously blind central area of the eye. “Where this dead retina was a complete blind spot, vision was restored,” said Dr. Frank Holz, the study’s lead author and ophthalmologist at the University of Bonn.
Surgical implantation begins with a vitrectomy—the removal of the gel inside the eye. The chip is then inserted under the retina through a tiny slit. Once healed, patients begin rehabilitation, gradually learning to interpret the new visual input delivered by the chip. This re-education is intensive, requiring hours of training over weeks or months.

Patients Regain Independence Through Vision
Though the restored vision is low-resolution and only in black and white—just 381 pixels—it has had a clear effect on quality of life. One year after surgery, many patients were able to read five lines lower on a standard vision chart. Everyday tasks like reading small labels, identifying objects, or working on crosswords became feasible again. “It’s not simple, learning to read again, but the more hours I put in, the more I pick up,” said Irvine.
As reported by NBC News, the device gave many participants a “clinically meaningful improvement” in vision—something previously unachievable for this patient group. Some did experience short-term side effects like elevated eye pressure or retinal bleeding, though most issues resolved within two months.
Crucially, the learning curve isn’t optional. Dr. Mahi Muqit, senior consultant at Moorfields Eye Hospital, emphasized that the implant is not a passive solution: “It’s not like you’re popping a chip in the eye and then you can see again. You need to learn to use this type of vision.” That process requires active participation and motivation from patients.


Behind the Chip, a New Neurotech Frontier
The implant is the brainchild of Dr. Daniel Palanker, a physicist at Stanford University, who spent years developing a design that would avoid wires and offer a minimally invasive path under the retina. His work reflects a growing intersection between ophthalmology and neurotechnology—an area now explored by Science Corporation, a California-based startup founded by Max Hodak, formerly of Neuralink.
According to The New York Times, next-generation versions of the chip are already in development, aiming to scale up from 400 to 10,000 pixels. These could allow for gray-scale vision and facial recognition. Early tests in animals have shown promising results, and new software is being written to refine visual perception through the chip.
Even with today’s limitations, the symbolic weight of the project is clear. “Think of this device as the pre-release iPhone,” said Dr. Demetrios Vavvas from Massachusetts Eye and Ear. “The limitations are clear. We shouldn’t oversell that the quality of life really improved. But there were certain [visual] tasks at which the patients were clearly better.”
For those who had resigned themselves to blindness, that difference is anything but minor. As Muqit put it, “Getting back the ability to read is a major improvement in their quality of life, lifts their mood and helps to restore their confidence and independence.”