When a person suffers a complex break near the top of the arm bone (the proximal humerus), the experience can be daunting for both the patient and the treating surgeon. Fortunately, modern medicine offers minimally invasive solutions, and one standout approach is anatomic proximal humeral nailing. Let’s break down why—and how—this technique continues to help people regain mobility and quality of life after injury.
Why Consider Proximal Humeral Nailing?
Surgeons often face tough decisions with severe shoulder fractures, especially when the bone is fragmented or the patient is older and has fragile bones. Here, anatomic proximal humeral nailing shines for a few main reasons:
- It’s less disruptive to soft tissues, helping keep blood flow intact for better healing.
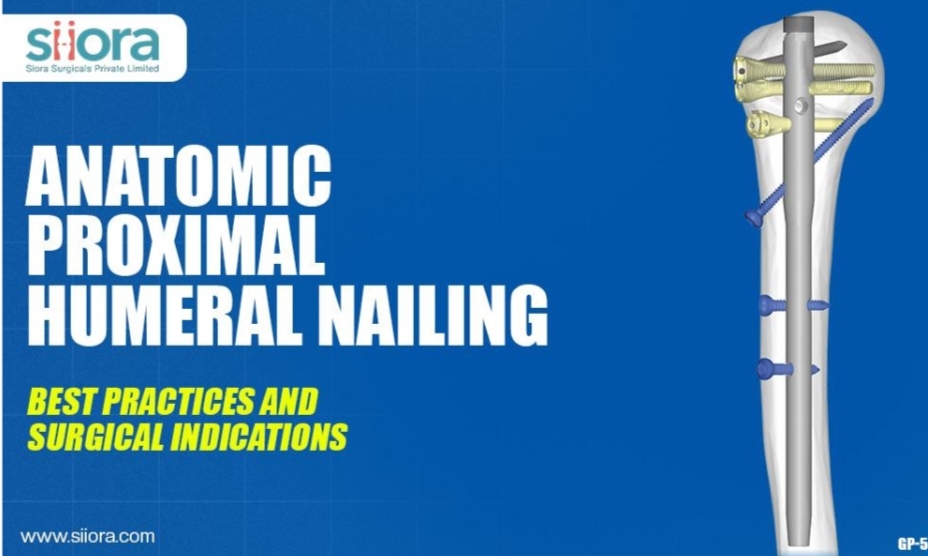
- The procedure uses a specially-designed nail set directly inside the bone, acting as a sturdy internal brace.
- It allows for early movement, which is essential for getting back daily activities and avoiding stiffness after injury, especially in older adults who want to stay independent.
When Is This Surgery the Right Choice?
Every patient’s situation is unique, but surgeons generally turn to proximal humeral nailing for cases where:
- Fractures are complex (especially those involving multiple parts of the bone near the shoulder).
- The bone fragments need help staying together but the head of the humerus is still viable.
- Patients may struggle with healing if more invasive surgery is used, or if non-surgical treatment carries risks of chronic pain and poor function.
- There’s a need to preserve shoulder function—think of a retired grandparent who enjoys gardening, or a younger person hoping to return to work or sports.
Surgeons must also consider bone quality, overall health, and the patient’s goals. These conversations matter; people want to know what their recovery will mean for their own lives.
Surgical Best Practices: What Really Matters
Caring for people means blending technical skill with genuine empathy. When performing anatomic proximal humeral nailing:
- The patient is carefully positioned (typically half-sitting) so the surgeon can access the shoulder easily and keep everything in natural alignment.
- Short, precise incisions minimize muscle and tissue trauma. As much healthy tissue as possible is spared.
- Temporary pins hold the bone fragments together while the surgeon prepares the nail’s pathway. The placement matters—a millimeter off can affect movement and pain down the line.
- Real-time X-ray imaging (fluoroscopy) helps guide every step, ensuring the final result is stable, secure, and as close to the person’s original anatomy as possible.
- Once the nail is set, locking screws keep bone pieces tightly anchored. Surgeons take extra care not to injure nerves or the joint surface.
Successful surgery isn’t just about technique. Surgeons need to talk patients through what’s happening and why, so they feel empowered to participate in their own recovery.
Pearls from Surgeons and Patients
Patients recovering from this surgery often say they appreciate rapid relief from pain and early movement in their arm. For surgeons, the key lessons are:
- Choose the right entry point for the nail—too high or too low causes complications.
- Double-check alignment to prevent loss of shoulder motion.
- Never rush fixing the tiny bone fragments, especially those where shoulder muscles attach.
Mistakes here can mean lingering pain or limited movement long-term.
Final Thoughts
Orthopedic implants like proximal humeral nailing isn’t just about fixing bones, it’s about returning people to their lives. With technical advances and compassionate care, patients with severe shoulder fractures can expect a smoother recovery and a brighter outlook on their future.